When we talk about cranial deformities, it is very important to differentiate positional craniofacial deformities from craniosynostosis, because the treatment and possible sequelae are very different.
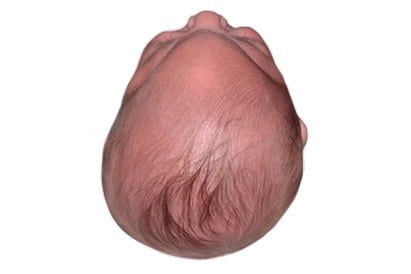
Craniosynostoses are due to the premature closure of some of the most important cranial sutures that allow the baby’s skull to grow as his brain grows.
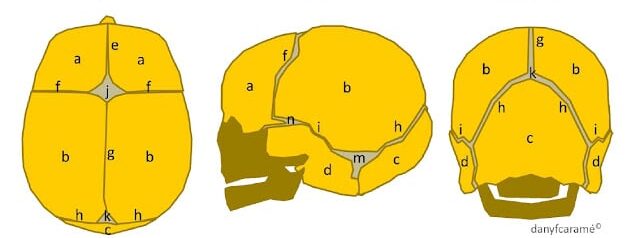
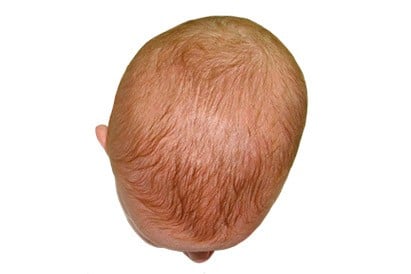
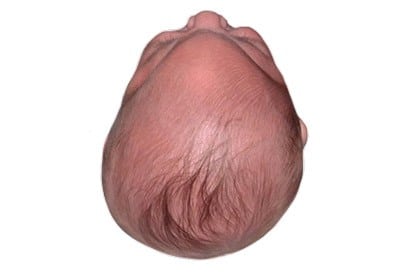
Compare the shape of your baby’s skull to the shape of a normal skull. See the different types of sutures and fontanelles:
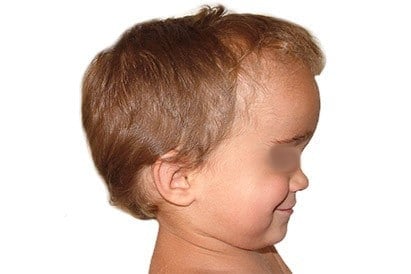
When a suture closes and the skull bones join together prematurely, the head will stop growing only on that part of the skull. Where the sutures have not come together, the baby’s head continues to grow. When this happens, the skull will be abnormally shaped, even though the brain inside has reached its normal size.
But, sometimes there is more than one suture that closes prematurely. In these cases, the brain may not have enough space to reach its normal size. This can cause a buildup of pressure inside the skull, which can cause problems such as blindness, seizures, or brain damage.
There are basically 4 types of craniosynostosis , based on the suture that closes prematurely:


The most frequent craniosynostoses in infants are:
Non-syndromic craniosynostoses present a high percentage of functional delays greater than 50%.
We invite you to read also this page about the consequences of untreated cranial deformities.
To confirm craniosynostosis, expert clinical diagnosis is necessary. Only in case of doubt (especially for the closed lambdoid suture) do we resort to skull X-rays.
To plan the surgical intervention, the practice of a three-dimensional helical scan (3D CT; 3D CT-scan) is useful. We reserve the use of Magnetic Resonance Imaging (NMR or MRI) for brain mass studies.
Before surgery we propose an ophthalmological review, neurological maturation test, dysmorphological pediatric study. Only in extreme cases is intracranial pressure (ICP) taken.
Depending on each case, a genetic study is requested, especially in complex or syndromic craniosynostosis (Crouzon, Apert, Saethre-Chotzen, etc).
For Oxycephaly, Trigonocephaly and certain types of scaphocephaly
The solution, if it does not occur spontaneously, requires surgery to avoid the problems that the brain malformation can cause in the normal development of the baby’s brain, with its possible physical and mental consequences.






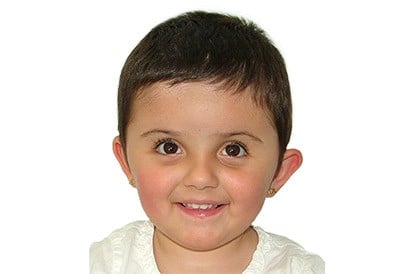

Cranial deformities should be treated as soon as possible (before 6 months of age). If they are not treated properly in time, they can trigger irreparable damage to the physical and mental development of the baby.
According to D. Marchac, on his article “Unoperated craniosynostosis patients: correction in adulthood“, “unoperated craniosynostosis creates a significant to severe disfigurement because of the frontal deformation. Therefore, only in mild cases can one propose a limited operation or an implant, avoiding an intracranial approach. In most cases, a radical intracranial approach is the only effective operation….

Experts in the diagnosis and treatment of skull deformities with DOC Band® method
INFORMACIÓN BÁSICA SOBRE PROTECCIÓN DE DATOS | |
Responsable | Dr. Joan Pinyot Garròs (en adelante, “European Craniofacial Medical Center”) |
Finalidad | Gestionar las solicitudes de diagnóstico inicial sobre deformidades craneales en bebés realizadas través del formulario web habilitado. |
Legitimación | Consentimiento del interesado/a. |
Destinatarios | No se cederán datos, salvo imperativo legal. |
Derechos | Acceder, rectificar y suprimir los datos, así como otros derechos, como se explica en la información adicional. |
Información adicional | Puede consultar la información adicional y detallada sobre Protección de Datos en este enlace. |
Antes de rellenar el formulario debe leer la información de nuestra política de protección de datos y nuestra condiciones de uso.
INFORMACIÓN BÁSICA SOBRE PROTECCIÓN DE DATOS | |
Responsable | Dr. Joan Pinyot Garròs (en adelante, “European Craniofacial Medical Center”) |
Finalidad | Dar respuesta a las solicitudes de contacto enviadas a través del formulario web habilitado. |
Legitimación | Consentimiento del interesado/a. |
Destinatarios | No se cederán datos, salvo imperativo legal. |
Transferencias Internacionales | No se realizan transferencias internacionales de datos. |
Derechos | Acceder, rectificar y suprimir los datos, así como otros derechos, como se explica en la información adicional. |
Información adicional | Puede consultar la información adicional y detallada sobre Protección de Datos en este enlace. |
You need to load content from reCAPTCHA to submit the form. Please note that doing so will share data with third-party providers.
More Information